It’s a life stage that 1.1 billion women worldwide will go through by 2025. So why are so many of us in the dark about menopause? Editor Trudi Brewer shares advances in hormone replacement therapies, her journey, and a hormonal stage that, for some, impacts every aspect of their lives.
Image BeautyEQ
Why is menopause a breeze for some and a bitch for others?
Women, by nature, share. Enjoy close friendships and are not intimidated by communicating their thoughts and feelings. We’re also resilient and, during our lives, experience the highs and lows that come with careers, motherhood and ageing. Discussions about pregnancy, birth, periods, and relationships are common - but not so much about menopause - why is that?
“With 1.1 billion women experiencing menopause worldwide by 2025, it’s time to shed the stigma attached to this significant hormonal shift that impacts every aspect of our lives - one being shame.”
I suspect that dates back to how our grandmothers and mothers dealt with 'the change.' Mine suffered from migraines, mood swings, and depression from what I believed was a failed marriage and the loss of her beauty and spirit. Fatigue and then the heartbreak of an empty nest didn’t help. Why has menopause historically been associated with the beginning of the end of a woman's youth and vitality? Or the start of her decline to irrelevance?
Transitioning from perimenopause to menopause happens over a decade for some women, and it can begin in your late 30s. It's a time when oestrogen levels, the essential female hormone, start declining. For some, it’s the start of hot flashes, mood swings, and irregular periods. Perimenopause can last for decades. But it's when you haven’t had a period for 12 months that it is the signal you are now in menopause. It’s also when women are at the peak of their careers, with busy, active lives.
As a journalist, I have covered every aspect of female-centric narratives, from sharing women’s career advice to beauty trends, wellness and cosmetic treatments. Menopause was never on my radar until a few years ago. It was also a subject I needed to be more knowledgeable about, which is odd because I am a woman in the thick of it. After researching and then finding an advocate for H.R.T. (hormone replacement therapy), an expert in women's health, I realised I had been let down for over a decade, at a time in my life when science-backed information and medical support were what I desperately needed. More on that later.
The changing attitude
Over the perimenopause years, women experience different symptoms, including insomnia, mood swings, depression, anxiety, brain fog, weight gain, joint pain, itchy skin, vaginal dryness, migraine headaches and pain during intercourse. That's not all; bone loss accelerates, and then there is pervasive dryness in the skin, nails, cuticles, throat, mouth, eyes, and thinning hair. Also, research has shown that oestrogen may help to protect the brain from Alzheimer's. Blocking some of the harmful effects of the amyloid-β protein, which build up and cause brain cells to become damaged or die.
In 2002, a landmark Women's Health Initiative (W.H.I.) published a game-changing article for menopausal women. That study found links between hormone replacement therapy and elevated health risks, such as breast cancer, blood clots, strokes and heart disease. Panic sent shock waves through the medical fraternity. In that one study, the average age of the participants was 63, and women primarily drove the risk assessments in their 70s; from that time, H.R.T. for women in their 40s and 50s was no longer recommended. In response to that study, medical schools quickly abandoned menopausal education. A 2017 survey sent to medical students across the U.S. found that 20 per cent had not heard a single lecture on menopause. A third of the respondents said they would not prescribe hormone replacement therapies to a symptomatic woman, even if she had no apparent medical conditions that would elevate risks. Potentially, those are the doctors working in our communities today.
After two decades of research, the initial scare tactics around H.R.T. and that study no longer stack up.
An article published on February 1st, 2023, in the New York Times, written by Susan Dominus, Women Have Been Misled About Menopause - got the world talking - loudly.
Today, there is positive science-backed research into hormone therapy that shows it can address most of the symptoms associated with menopause but can also decrease the risk of diabetes and protect the body against osteoporosis. It also helps prevent and treat menopausal genitourinary syndrome, a range of symptoms, including urinary tract infections and pain during sex, that affects nearly half of postmenopausal women. One of the biggest takeaways from that New York Times article by Susan Dominus was that age matters. For women who go through early menopause before the age of 45, hormone therapy is life-changing because they're at greater risk for osteoporosis if they don't receive hormones up until the typical age of menopause.
What is hormone replacement therapy?
From oral medication to transdermal patches, gels or vaginal treatments. The type of H.R.T. best prescribed varies depending on your age, health conditions, and if you have had a hysterectomy. If you still have your uterus, then often treatment combines oestrogen and progestogen. For a treatment commonly prescribed globally until that 2002 Women's Health Initiative (W.H.I.) study, new analyses of the data from that study, along with many other studies, have since given reassurance that the risks of hormone therapy are low. However, H.R.T. is still recovering from that reputation. According to Dr Stephanie Faubion, a women’s health expert at Mayo Clinic in Florida and the medical director of the North American Menopause Society, “The current official position is that the benefits of hormone therapy typically outweigh the risks for most healthy, symptomatic women under 60 and within ten years of menopause onset.”
Today’s formulations mimic the natural hormones in a woman’s body, such as Bioidentical Hormone Replacement Therapy, available and funded here in New Zealand. There are also new methods of delivery: Taking hormones via a transdermal patch rather than a pill allows the medication to bypass the liver. According to Rebecca Thurston, a professor of psychiatry at the University of Pittsburgh who studies menopause, “About 85 per cent of women experiencing menopausal symptoms have been underserved.” An oversight that she considers one of the great blind spots of medicine. “It suggests that we have a high cultural tolerance for women’s suffering,” Thurston says. “It’s not regarded as important.”
Hormone therapy has risks, as does any medication that helps relieve pain or discomfort. There have been dozens of studies since that first 2002 W.H.I. study to prove its efficacy. If the symptoms of menopause are affecting your life and happiness, my experience now I am on H.R.T. (and its early days) is that the benefits of taking hormones under the guidance of a good G.P. well outweigh the risks.
My menopause journey
Starting perimenopause in my mid-40s, my symptoms were mild at first, and I never really thought about it. I have always been a light sleeper; who isn't after having kids? I put my mood swings down to fatigue and my perfection complex. But brain fog, as well as a patchy libido and irregular periods, were worrying. After insisting on a blood test, it confirmed I was in perimenopause by my doctor (a doctor I had been going to for over 30 years), who, when I quickly suggested H.R.T., promptly refused me. My reluctant male GP, who scheduled 10-minute appointments if I was lucky enough to get one during COVID, was a great family doctor (now retired); he guided me through my life from my 20s to my 40s, including the birth of my two sons. I trusted him. He was calm, considerate and caring. But I now know his knowledge of menopause was lacking. He never had the time to share the risks and benefits of H.R.T., which could work for my constant insomnia, waking at 3 am, followed by anxiety. Not to mention dry, itchy skin and loss of libido. So, sticking with that age-old research and a brief dismissive discussion on the risks of breast cancer with H.R.T., he offered anti-anxiety medication that would also help me sleep. I revisited the H.R.T. discussion several times and received the same rhetoric. It wasn’t until he retired and a young female Australian doctor replaced him that I brought up the same conversation around H.R.T. She said, “It’s too late; you should have been on H.R.T. in our early 40s. Just keep taking that anti-anxiety medication you have been prescribed.” That was the motivation I needed to find a new G.P.
Where do you find the best menopause advice?
Suppose there was a superabundance of research into menopause, a life stage as inevitable as ageing. Suppose women did not find themselves apologising for those symptoms at work or experiencing angry outbursts or tearful mood swings at home. Imagine asking your doctor repeatedly for H.R.T., a request that, in my case, fell on deaf ears. I suggest (from experience) that if your doctor isn’t discussing hormone therapy with you, it’s not because it’s not available. It may be because of gaps in their knowledge.
Today, women in their 40s and 50s are dynamic. Career-driven, keen to stay youthful and fit and enjoy all aspects of their life, including relationships. They are engaged and have much to bring to our society. At every life stage, there are hurdles to overcome. We all have or have not had menstruation issues. However, some women experience mood swings that prevent them from functioning; we call that premenstrual syndrome (P.M.S.). Motherhood, which some of us embrace and relish, and others suffer postpartum depression, which is debilitating. But until now, menopause has been a discussion that is not that easy to have, and so many women suffer to the point of breakdown.
Dr Gunter, obstetrician and gynaecologist and the author of “The Menopause Manifesto” and “The Vagina Bible.” Once said, “Menopause has long been treated as a pre-death, a metamorphosis from a woman to a crone with her exit ticket already punched. This is because a woman’s worth was measured by her reproductive ability and, by extension, her femininity, as defined by a narrow, misogynistic standard.”
Expert advice
Dr Antje Bongartz
Being misdiagnosed with anxiety or depression rather than being offered H.R.T. as a treatment for perimenopause is common. When I saw Dr Antje Bongartz at Takapuna Health, there was finally a light at the end of a very frustrating, narrow tunnel. Her extensive knowledge and validation that I had not been given, along with the best options for my symptoms, compelled me to share my journey and what I have learned. Here, Dr Bongartz conveys some of the most commonly asked questions we should be discussing.
Q&A
What age do women typically hit perimenopause and then full menopause?
There is a considerable variation in the onset of perimenopause between 35 and 58 years. Still, most women start with first symptoms around 50 and will have their most symptomatic years between 52 and 55 years.
Does menopause differ in women who have not had children?
Some studies have found that women who had an early onset of periods and who never had children might have a two or three-fold higher risk of early onset of perimenopause.
What are the symptoms, common and uncommon?
The most common symptoms are night sweats, hot flashes, brain fog, anger, and itchy skin. Muscle and joint pain, loss of bone density, hair loss, ageing skin, and abdominal weight gain are less common as initial symptoms.
How can weight gain be managed?
Abdominal weight gain is usually a slow onset symptom but does happen to most women due to the declining oestrogen. Weight gain can be managed by conscious eating, avoiding too many refined carbs, sometimes time-restricted eating, and a healthy lifestyle with sufficient exercise, recreation, and stress avoidance. It sounds easy, but it isn't. Most women in their 50s have a demanding job and family situation. Finding time for exercise and recreational activities and providing a healthy diet can be a challenge.
What about H.R.T.? So many doctors are against this treatment. Why?
The initial H.R.T. in the 1990s was very unsafe for women regarding cardiovascular and breast cancer risk, but this was first apparent to medical professionals due to the Women's Health Study after some years of treatment. It came as a massive shock for doctors and women who stopped H.R.T. usage for some time. Many health professionals are still stuck in this belief and are not up-to-date with current treatment options and safety data, so they discourage women from starting treatment.
How has H.R.T. changed since the 1990s?
Health professionals initially used synthetic or animal-derived hormones, which caused a significantly higher cardiovascular risk. For example, pharmaceutical companies extracted oestrogen from pregnant horse urine, which had a 400-fold more increased blood clotting risk compared to human oestrogen. So, women were getting strokes and heart attacks. The synthetic hormones, especially progesterone, were blocking the receptors in the body for weeks, which led to a higher breast cancer risk. The current bio (body) identical H.R.T. has reduced these risks significantly.
What are bioidentical hormones?
Nowadays, laboratories manufacture bio (body) hormones from plants. They have the same chemical structure as our hormones and the same benefits and risks.
What is the best age to start and stop taking H.R.T.?
The best age to start HRT is the beginning of perimenopause. It can be different for women; some start in their 40s or even earlier, and most will begin around 50. It is essential to start H.R.T. in the 50s, as this will most benefit our metabolic health, keeping cholesterol in check and reducing our cardiovascular risk. Usually, this only happens when one starts H.R.T. before the 60s.
Do supplements help? If so, what are the best options?
Some well-researched supplements, such as black cohosh, have been used for many years to help with perimenopause symptoms. They usually are effective for a particular time and then can lose their effect. One must check the liver function, as some can affect it negatively. Other strategies in early perimenopause are supplements to detox high oestrogen levels, such as DIM and Sulforaphane. These can be helpful for the initial phase.
Why do women lose their libido during menopause?
The loss of libido that many women suffer is a multifactorial problem. It is caused not only by declining oestrogen and testosterone levels but also by psychological and social stressors. Women are in a demanding phase of their lives, and stress has a very negative impact on libido. They are often losing confidence due to the changing body, which can negatively affect their attitude towards intimacy.
What's the best way to get it back?
The first approach is to be aware of the changes and optimise lifestyle, sleep, stress, exercise, and diet. It is essential to initiate healthy ageing early in the 50s. Depending on the individual symptoms, HRT with oestrogen, progesterone, and testosterone cream (Androfeme, which is available but not funded in New Zealand and costs $153), can significantly support a woman's well-being and libido.
New technology
When you think about Clearblue, at-home pregnancy and ovulation tests spring to mind; however, their latest launch is all about menopause. Determined to turn up the volume on the conversation around menopause, this new test addresses an often overlooked and underfunded sector of women’s health. The new Clearblue Menopause Stage Indicator is a one-of-its-kind testing kit that measures your follicle-stimulating hormone levels (FSH) with five urine test strips you use over ten days. Along with a Clearblue menopause app, this goes beyond just averaging your test results; you can then continue to use the app to record symptoms you might be experiencing to provide insight into where you are in your menopause journey.
A Great Guide
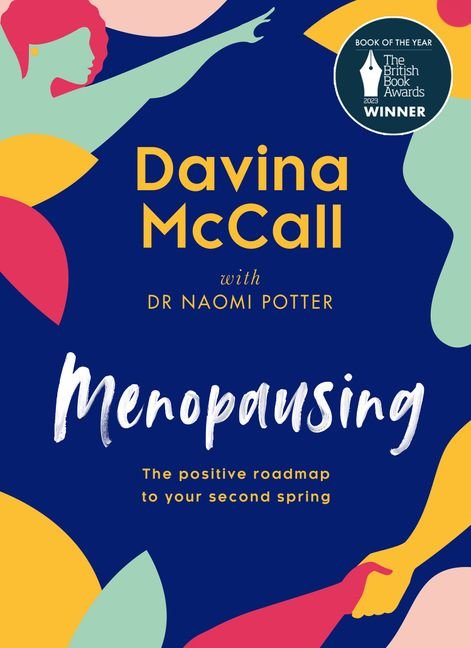
British TV presenter Davina McCall (famous for TV Shows including Big Brother, Masked Singer and Masked Dancer in the U.K.) and her 2021 B.B.C. documentary series Sex, Myths and the Menopause, available on TVNZ+ on-demand, is helping normalise the menopause conversation. She has helped demystify the midlife taboos, including H.R.T. and sex. Her latest project, a book, ‘Menopausing’ recently won the British Book of the Year in 2023, co-written by British menopause expert G.P. Dr Naomi Potter, who is the founder of dedicated Menopause Care clinics in the U.K. This guide to life in menopause, with evidence-based science and honest, no-holds-barred advice, is brilliant. McCall’s funny, oversharing style ("I got a blister on my labia," she says in the intro) shares how talking openly about menopause has helped her better understand what is going on to her and millions of other women. This book charts McCall's experience, including how terrifying it is that so many women get prescribed antidepressants when presenting quite clearly with menopausal symptoms to their G.P.s. Dr Potter adds sound scientific advice, and together, they have created a great read, a positive roadmap to your second spring.
Skin and menopause
When it comes to the symptoms of menopause that affect your appearance, there is a groundswell of high-profile, well-funded menopause-related beauty products, as well as a growing list of celebrities willing to admit it’s happening to them. Here’s how to understand what maturing skin needs to stay looking vital.
You can have youthful-looking skin without surgery
That age-old defeatist attitude towards menopause means many women believe that youthful, glowing skin is impossible to achieve without cosmetic medicine or surgery. It is possible to keep your skin in great shape during and after menopause using targeted ingredients. Dr Des Fernandes, founder of Environ skincare, led research into the effects of menopause on women's skin, "Oestrogen plays a role in stimulating collagen production and glycosaminoglycans such as hyaluronic acid. The decline of progesterone contributes to the deficiency of the skin's natural oils, and together, these compromised moisture components leave the skin susceptible to transepidermal water loss."
Other skin symptoms during menopause include flushing, rosacea, and hormonal acne. Then, the skin loses collagen, the cushion it needs to bounce back after laughing or even blinking, which is when you start to see wrinkles. The good news is that science has transformed skincare ingredients and their efficacy. Certain ingredients will improve the skin's health, smoothness and all-round radiance.
These include hyaluronic acid, peptides (proteins), niacinamide (vitamin B3), and vitamin A (retinol), which help improve skin cell turnover, which also naturally declines with age. Vitamin A is the most potent promoter of collagen and natural moisturising factors. As the pioneer and leading specialist in vitamin A skin science, Dr Fernandes maintains that the topical replenishment of vitamin A and antioxidants is the most effective starting point for women experiencing the effects of menopause on their skin. "The most important nutrient for skin before, during and after menopause is vitamin A. This essential skin nutrient controls the normalised activity of skin cells through its effects on cellular DNA, promotes the healthy metabolism and differentiation of skin cells, and is the most powerful promoter of the skin's natural moisturising factors." Vitamin C also has many benefits, including collagen stimulation and skin brightening. Ceramides (lipids that nourish the skin) and vitamin E nourish ageing skin.
Dry skin can be hydrated
Younger women often overlook skincare geared towards mature skin for obvious reasons. Still, they can also benefit from more youthful skin, and starting a good routine in your 30s is essential to keep your skin looking its best for life. When you add a skin serum to your routine, you'll notice the increased hydration and firmness, which allows for smoother makeup application - an ageless benefit. Hyaluronic acid and other powerful peptides also contribute to purging bacteria from the skin, which can be helpful for acne. Also, many of the ingredients listed protect and strengthen your skin's natural microbiome (its barrier), keeping moisture in and irritants out, another bonus to keeping skin looking younger for longer.
Wrinkles and menopause don’t have to go hand in hand
Dry skin is wrinkled skin. Fact. But dry skin can affect anyone at any age, especially with lifestyle, diet and climate in the mix. As oestrogen levels fall, skin becomes thinner, retains less moisture, appears dull or transparent and bruises quickly. Oestrogen is the skin's natural hydration booster, facilitating the production of ceramides, natural hyaluronic acid, and sebum (naturally produced oil). So, to keep your skin looking firm and nourished, you need to flood the skin with moisture and always wear an SPF to protect it. Dr Fernandes's skincare-led consumer research revealed that despite experiencing significant changes to skin during menopausal phases, 66 per cent of women do not seek professional skincare advice or treatments to assist with these skin concerns. When asked what the most visible effects of perimenopause or menopause are on the skin, 51 per cent of respondents stated dry, itchy skin and over 34 per cent cited wrinkles, sagging and loss of volume. One in five respondents suffered acne flare-ups. When asked how respondents felt about the effects of menopause on their skin, only 13 per cent were accepting of it. The overwhelming majority used ‘sad’, ‘awful’, ‘embarrassed’ and ‘frustrated’ descriptors. Some women even felt the need to ‘cover-up’ and that their skin made them feel unattractive and depressed. "Skincare professionals can help greatly by providing personalised expert recommendations on home skincare and professional treatments," says Dr Fernandes. "Menopause is as individual as a person's genetics when it comes to the symptoms and effects on the skin, which makes personalised advice even more important."




















Here is a guide, and the brands worth buying.